People all over the world are struggling to breathe because of respiratory infections and chronic diseases. But further damage may be prevented by matching the right treatments to the right patients. Here, experts explain why a preventative patient-centred approach is key to transforming respiratory care – and taking the pressure off struggling health services.
The Covid-19 pandemic highlighted the enormous toll respiratory diseases take on the health and wealth of populations. Yet even before, illnesses that affect the lungs were a leading cause of hospitalisation. Millions of hospital beds are filled every year due to seasonal influenza, pneumonia, and RSV, to name a few.
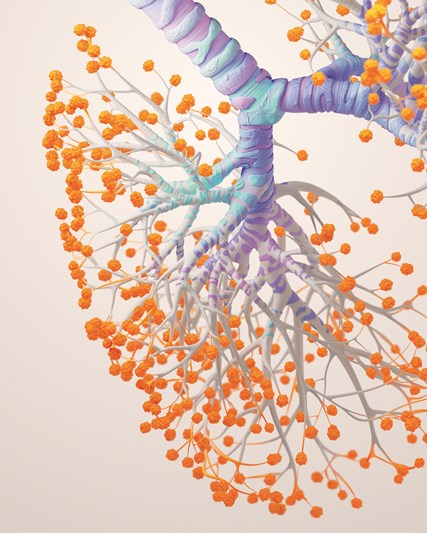
Chronic lung diseases create an even bigger burden. Every year, more than three million people die due to chronic obstructive pulmonary disease (COPD), making it the world’s third leading cause of death. Recent data suggests that 262million people have asthma, around a quarter of which suffer from severe asthma. And the picture is worsening: between 1990 and 2017, the number of people worldwide with a chronic respiratory disease rose by 40% to nearly 550 million (PDF - 1,960KB).
“I don’t think anyone can plead ignorance about the importance of the lung post-Covid,” says Tonya Winders, President and CEO of patient advocacy organisation the Global Allergy and Airways Patient Platform.
“Respiratory disease is certainly on the rise, acute and chronic, keeping people from breathing freely and fully. This is a public health crisis we can no longer ignore.”
The good news is a significant proportion of respiratory infections, which can lead to disease, are preventable. Intervening earlier may change the trajectory of chronic respiratory disease by averting flare-ups that weaken the lungs and hastening deterioration.
“That’s why prevention is so important,” says Dr Eduardo Genofre, Vice President, Respiratory, Global Medical Specialty Care at GSK.
“In some individuals with a baseline condition, an infection hits and boom, they have a permanent condition. Some of the biology changes, and from that moment on, the immune system is operating in a different way.”
Taking a preventative, patient-centred approach, says Winders, rather than a one-sized fits-all solution, is key to solving the problem.
“Genetics, environment, early intervention, vaccination: all these different pillars set one up for a lifetime of lung health rather than waiting until someone is ill.
“They don’t want to be patients. They want to be people.”
Putting patients first
With growing insight into the biological drivers of chronic respiratory conditions, medical treatments are moving beyond a one-size-fits-all model to find treatments that take aim at underlying causes in individual patients.
New therapies have the potential to act on short-term symptoms and also improve the long-term outcomes by modifying the course of disease, slowing disease progression and in some cases, potentially preventing the worst symptoms, like exacerbations (lung attacks), from occurring in the first place.
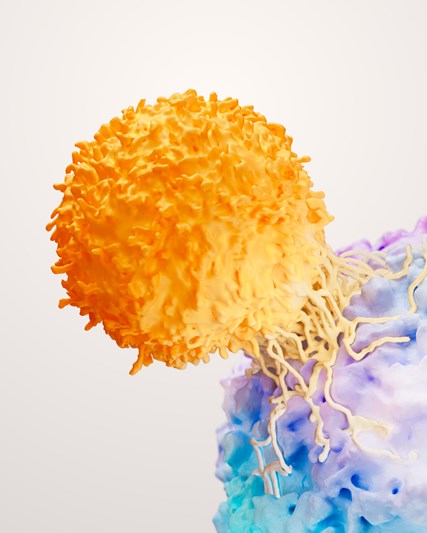
Today, scientists better understand the role the immune system plays in chronic conditions such as COPD and asthma, and how targeting specific immune drivers with precision medicines could change the trajectory of chronic diseases. Because different parts of the immune system are implicated in different patients, these medicines need to be paired with the right patients in order to maximise the benefits.
For example, some types of asthma can be identified by a blood test that measures levels of a white blood cell known as an eosinophil. By identifying the type of asthma and the immune pathway involved, a doctor can select the most appropriate, evidence-based treatment for that patient. This could make new treatment goals such as clinical remission possible.
“It’s an exciting time for research in respiratory disease,” says Kaivan Khavandi, Senior Vice President of Respiratory and Immunology R&D at GSK.
“We are just scratching the surface when it comes to targeted therapies that get at the underlying drivers of disease in different people.”
Peace of mind
Another important area of innovation is making treatments more convenient. Many immune-targeting treatments for asthma are typically administered by a clinician in a doctor’s office, but researchers, including those at GSK, are developing new medicines that can be taken at home by self-injection. They are also working on long-acting versions of treatments that can be given every six months.
“People living with a respiratory disease don’t need to be reminded every month or every day that they are sick, that they have that disease,” says Dr Genofre.
“[Long-acting treatments] will give them some peace of mind – they can live their lives without thinking about their condition.”
Furthermore, treatments that ward off symptoms can improve the day-to-day quality of life for people with severe respiratory disease – and can even change the course of disease.
Chris Compton, VP of Inhaled Medicines at GSK, says: “Once daily treatments, in easy-to-use inhalers, provide the opportunity to optimise the treatment of patients earlier, so reducing the risk of exacerbations, improving symptoms and ultimately enabling disease stability.”
Cutting down or eliminating flare-ups such as asthma attacks may reduce long-term damage to the lungs, which in turn slows down disease progression. It also limits the patient’s reliance on oral corticosteroids, a rescue medication for emergency situations, the repeated use of which can cause unpleasant side effects such as weight gain, sleep disturbances and anxiety.
The air we breathe
For some, those same rescue medications they use to protect against lung damage are also impacting the environment.
Metered dose inhalers (MDIs) use a propellant that helps push the medicine out of the inhaler and into the lungs. However, the current propellants in MDIs significantly contribute to global warming.
GSK is currently progressing with clinical trials to transition one of its inhalers to a next generation, lower carbon propellant which, if successful, will reduce the company’s emissions by approximately 90%. This will supplement their existing range of low carbon, propellant-free dry powder inhalers (DPIs) to help protect the health of people and the planet.
“We support efforts to increase the use of DPIs, where clinically appropriate,” Compton says. “There are instances, however, when the use of MDIs is medically necessary or preferred by the patient.”
Climate change in itself poses a threat to respiratory health by increasing things like pollen count and creating better conditions for infectious pathogens – disease-causing organisms – to thrive in.
Common pollutants, such as those emitted from vehicle exhausts, irritate the airways, sometimes with fatal results. It is estimated that air pollution is responsible for around 7million premature deaths every year due to ischemic heart disease, stroke, COPD, lung cancer and acute respiratory infections.
Putting resources into cleaning up the atmosphere is therefore a respiratory health necessity. WHO and other agencies have called for cities and people to bring air pollution to safe levels by 2030 to protect human health.
Staying ahead
When it comes to respiratory disease, preventing patients from getting infections – and reducing disease deterioration – is just as important. Not only does this make sense for patients, but for their caregivers, health systems and economies more broadly.
COPD alone is predicted to cost the global economy around $4 trillion between 2020 and 250 in lost productivity, the cost of treatment, and the taking up of hospital beds for days, sometimes weeks at a time.
The Global Initiative for Chronic Obstructive Lung Disease recommends (PDF - 330KB) that COPD patients stay up to date with vaccinations against a range of infectious diseases – particularly seasonal viruses.
Severe respiratory infections can cause lasting damage to lung tissue, worsening the symptoms of chronic conditions. To help get ahead of these types of infections, GSK has developed a robust vaccines portfolio specifically designed to help those most at risk.
“It really has only been in the last decade that prevention is on the table and the last two-to-three years that it is taking a more central focus,” Winders concludes.
“That provides a lot of hope.”