Scroll to explore
Ahead Together in genetics/genomics/vaccines/medicines/innovation
How our R&D approach helps us get Ahead Together
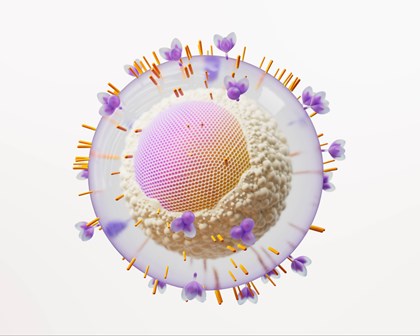
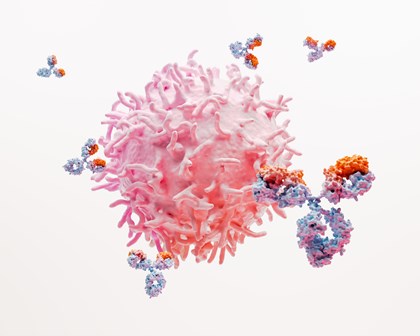
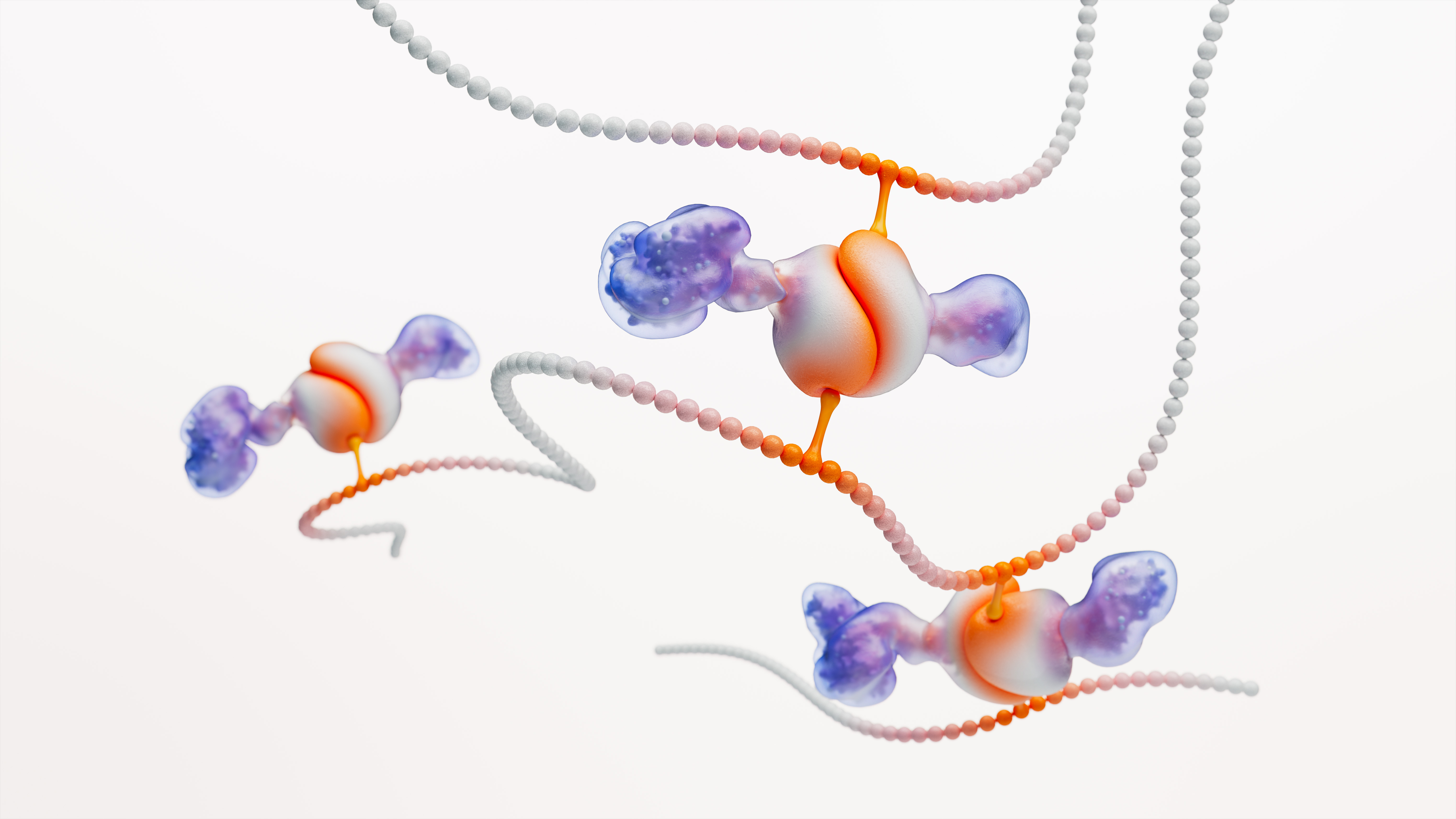
We’re combining the power of genetic and genomic insights into what causes disease, with the speed and scale of artificial intelligence and machine learning (AI/ML) to make better predictions about who a treatment might work for, and why.
We believe this powerful combination of data and technology holds the key to fundamentally transforming medical discovery for the better, improving R&D success rates and shaping how even the most challenging diseases, like neurological conditions and cancer, can be both prevented and treated.
There’s never been a time when science and technology have formed such a powerful union as they do now. We’re able to identify drug discovery targets using genomics and AI/ML in a way that is unprecedented. We’re also able to use more approaches than ever before to design new vaccines and medicines to address the root cause of disease.
-
Our R&D investment in 2023
£6.2bn -
Major business development deals in 2023
6 -
Vaccines and medicines in the pipeline
71 -
Phase I programmes started in 2023
8
Watch how we innovate

Spotlight on GSK innovation
Our pipeline
As a global biopharma leader, we invest heavily in our industry-leading pipeline of potential vaccines and specialty medicines that help us to get ahead of disease together
Therapeutic areas
The four areas of human health we focus on to get ahead of disease are: infectious diseases, HIV, respiratory/immunology, and oncology. We remain open to opportunities outside these core areas where the science aligns with our strategic approach.
Innovation events and conferences
Hear from industry experts, explore the latest breakthroughs and network with us.