Most patients hospitalised with chronic obstructive pulmonary disease (COPD) are readmitted within a year and typically enter a spiral of decline in lung function, overall quality of life and survival. Here, Dr Kaivan Khavandi, SVP of R&D for Respiratory, Immunology and Inflammation at GSK, explains why we can’t afford to ignore these outcomes – and how his team aims to prevent them.
Almost all physicians have experienced the distress of a COPD patient presenting with an exacerbation – gasping for air as their airways constrict.
I have clear memories of treating these patients from my own time working in emergency and acute medicine in a large tertiary hospital in London. Each patient is unique, both in their journey and the underlying disease processes at play, but they are united at this moment in their concern and fear, and their expectant expressions at the nurses and doctors to help them.
However, despite our best efforts with bronchodilators and steroids, some patients fail to improve, leading to hospitalisation, intensive care and sometimes mechanical ventilation. These situations have the same level of urgency as a heart attack or a stroke. Many people don’t realise how serious these events can be.
The numbers are striking. 1 in 10 patients hospitalised with COPD never leave the hospital, and almost 90% face re-admission within the year. COPD is projected to become the leading cause of all hospital admissions and poses a significant cost to health systems globally, with an estimated $4 trillion to be spent on factors like hospital stays by 2050. This is why we take this disease so seriously.
While these statistics are staggering, they do not come close to capturing the true impact to patients. My role has shifted from physician scientist and academic researcher to therapeutic discoverer and developer, but my unilateral commitment to positively transform patient care is unchanged. To truly conquer this disease, we must deeply understand it at both the population and individual level. Our research is therefore driven by a dedication to uncovering the underlying drivers of COPD, paving the way for genuinely personalised solutions.
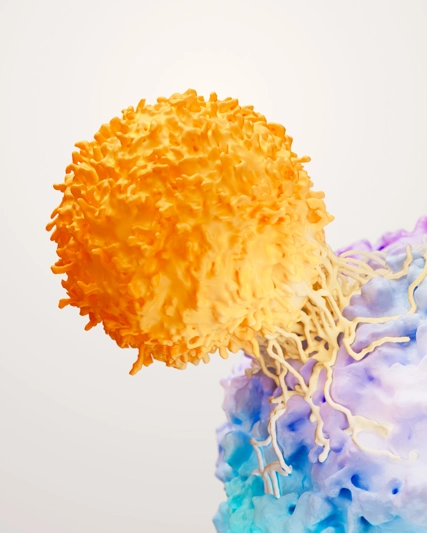
COPD, encompassing chronic bronchitis and/or emphysema, presents a spectrum of challenges. Inhalers offer important relief from airway constriction, but treatments targeting the underlying inflammation associated with COPD are still emerging. The key lies in recognising the heterogeneity of the disease – understanding that COPD isn't a single entity but a collection of individual traits. By harnessing this, we can better match treatments to the specific needs of the patient.
GSK has been at the forefront in COPD research and has pioneered the understanding of certain underlying drivers of the disease. This insight has led to more targeted approaches to treating COPD, moving beyond one-size-fits-all solutions to advance care that can address the root causes of disease. We were the first to apply this understanding in COPD research and we’re also researching longer-acting therapeutic approaches for this disease.
Even with these advancements, considerable variations still exist among COPD patients, and in turn, their outcomes. Factors like genetics and environmental influences cause differing phenotypes or observable traits (for example, markers in the blood or exacerbation risk) which affect treatment response. Consequently, identifying these phenotypes allows us to target these underlying processes and optimise the effectiveness of treatments.
Advanced technology is key to unlocking further innovation in COPD and helps us to understand on a deeper level these unique disease characteristics. For example, we use extensive datasets derived from diverse sources (for example, clinical trials, integrated with groups of patients that have been monitored over years, to understand disease progression) combined with technologies, like cell-atlassing, which are designed to map the cellular basis of a disease. AI and machine learning are then used to reason over these complex, integrated datasets, identify patterns and associations that may be challenging to spot through traditional analyses, and then predict how novel treatments can work for different patients.
This has helped us develop therapeutic approaches that target two separate but contributing pathways to more completely address the disease based on patients' phenotypic traits – observable and measurable characteristic traits that result from an interaction between a patient’s genetics and the environment. There’s so much more to be understood and opportunity to innovate in this space and I’m profoundly motivated to drive GSK to continue to be at the forefront of such advances.
We are meticulous in our approach, keeping patients at the heart of what we do and considering their lived experience, the effects of their disease, and what they truly need from new medicines. Our history, expertise, and deep scientific knowledge are driving real innovations in COPD.
Patients, their caregivers, and healthcare systems depend on it, and I am proud of my team’s dedication to collaboratively advance and improve treatment in this area.